An article by Consultant Physiotherapist and Sonographer, Dr. Jeremy Lewis
Jeremy Lewis PhD FCSP MMACP
Consultant Physiotherapist, Central London Community Healthcare NHS Trust, London, UK; Professor of Musculoskeletal Research, Faculty of Education and Health Sciences, University of Limerick, Ireland; Reader in Physiotherapy, School of Health and Social Work, University of Hertfordshire, Hatfield, UK; Sonographer
Introduction
Rotator cuff (RC) tendinopathy refers to the clinical presentation of pain and weakness present in the shoulder and generally, but not exclusively, experienced during external rotation and elevation, once other causes of symptoms have been excluded (Lewis 2009). The true prevalence and incidence of symptomatic RC tendinopathy remains undetermined due to the lack of certainty between clinical symptoms and RC structural failure. Those clinically diagnosed with RC tendinopathy should have considerable confidence that graduated and supervised exercise has at least equivalent outcome to surgical intervention, with the added generalised benefits of exercise http://www.youtube. com/watch?v=aUaInS6HIGo, a faster return to work and at a lower cost than surgery. This evidence relates to those diagnosed with subacromial pain syndrome (Lewis 2011), rotator cuff tendinopathy (Holmgren et al 2012) and atraumatic partial and full thickness rotator cuff tears (Kuhn et al 2013, Kukkonen et al 2014). Evidence also exists for significant benefit of exercise in those with massive inoperable RC tears when compared to placebo treatment (Ainsworth et al 2009). This body of evidence conflicts with reports of a 750% increase in subacromial decompressions performed in the United Kingdom between 2001 to 2010 (Judge et al 2014) and a 600% increase in arthroscopic RC repairs performed in the United States between 1996 to 2006 (Colvin et al 2012), and highlights the need for carefully thoughtout care pathways for these conditions, determining thresholds for when other interventions, such as injection therapy and surgery should be considered.
The rotator cuff is commonly described as a group of muscles and tendons that are recruited equally and synchronously during shoulder movement to stabilise the humeral head on to the scapula. This precept has been challenged. The supraspinatus and infraspinatus are recruited at higher levels during shoulder flexion, and concomitantly the subscapularis is recruited at higher levels during extension. This varying pattern of recruitment was also shown not to be load dependent (Wattanaprakornkul et al 2011a). The asynchronous action of the RC potentially may be used to inform clinical exercise management.
It is important not to assume that observed structural failure in the RC tendons is always symptomatic. Frost et al (1999) reported that people with and without symptoms of RC tendinopathy demonstrated equivalent RC pathological changes. Asymptomatic professional baseball pitchers demonstrate substantial RC pathology in their pitching and catching shoulders (Miniaci et al 2002) and, more recently, ultrasound studies of men without symptoms identified structural changes in 96% of those scanned including subacromial bursal thickening, supraspinatus tendinosis and partial thickness tears, as well as labral pathology (Girish et al 2011). In most cases the onset of RC tendinopathy is associated with increased load on the RC structures. Increased load is a very relative term varying between individuals, as well as within an individual during periods of variations in activity level. Genetics (Harvie et al 2004) and lifestyle (Dean & Söderlund In Press-a) are factors that may contribute to RC tendinopathy.
Tendon pathology has been described as a continuum (Cook & Purdam 2009; McCreesh & Lewis 2013; Lewis 2010), and while loading is essential for tendon production, both chronic under-load and unaccustomed overload may have a potential detrimental impact on tendon health structurally. Loading may therefore be subcategorised into adaptive load that results in the synthesis of healthy tendon, and mal-adaptive load that may be detrimental. As mentioned, lifestyle and other factors may also positively or negatively influence tendon quality and there may be a threshold of complex factors that favours tendon production or degradation. Reasons why some people experience pain as well as the source of the pain remain uncertain. Tendon, bursa, osteotendinous junction and musculotendinous junctions, capsular tissues and muscles, and their attendant nerve supply, are all potential sources of local pain. Central sensitisation (Paul et al 2012; Coronado et al 2014) and cortical changes (Ngomo et al 2014) may also be involved and this may influence assessment findings and outcome. Corticospinal excitability of the infraspinatus muscle was found to be decreased on the affected side and this change was associated with pain duration but not intensity (Ngomo et al 2014).
Assessment
Special orthopaedic tests have been developed to clinically diagnose RC tendinopathy. However, narrative and systematic reviews (Lewis & Tennent 2007; Hegedus et al 2012; Hegedus & Lewis 2014) have challenged the certainty that these tests can diagnose RC tendinopathy with the clinical assurance required to inform clinical decision making. Needle EMG has demonstrated that during the full and empty can test the supraspinatus is activated. However, eight and nine other muscles were respectively reported to be equally activated during these procedures (Boettcher et al 2009), a finding that challenges the usefulness of these tests other than one of symptom reproduction. Imaging, most commonly ultrasound and MRI, and the intra-operative visualisation of structural failure are procedures commonly used as the gold standard comparators to determine the accuracy of the clinical tests (Michener et al 2009). However, the ability for observed structural failure to determine the usefulness of clinical tests is substantially challenged, as multiple studies have demonstrated a poor relationship between imaging and symptoms (Frost et al 1999; Sher et al 1995; Milgrom et al 1998; Girish et al 2011). Further discussion, and the reasons for this disparity, has been published (Lewis 2009, 2011) and these data suggest that many people will undergo surgery on tissues that may not be associated with the presenting symptoms. The diagnostic uncertainty of the clinical tests and imaging procedures to confirm a diagnosis or identify which tissues are responsible to the individual’s symptoms has prompted some to use treatment direction tests to guide patient management. One such procedure, the Shoulder Symptom Modification Procedure (SSMP) (Lewis 2009), was developed to determine the influence of thoracic and scapular posture as well as the relationship of the humeral head to the glenoid fossa on the patient’s symptoms. A diagnosis of RC tendinopathy is reached if these procedures do not alleviate the individual’s symptoms. This type of approach requires validation.
Management
Once diagnosed it may be beneficial, clinically, to subcategorise the presenting symptoms and offer management appropriate to the stage of RC tendinopathy. Subgrouping has been advocated for those suffering from low back pain as a method of improving clinical outcome (O’Sullivan 2005) and this may also benefit those with RC tendinopathy instead of a “one size fits all” approach. Figure 1 details a suggestion for the possible stages of RC tendinopathy.
Figure 1: Model for the onset and management of RC tendinopathy
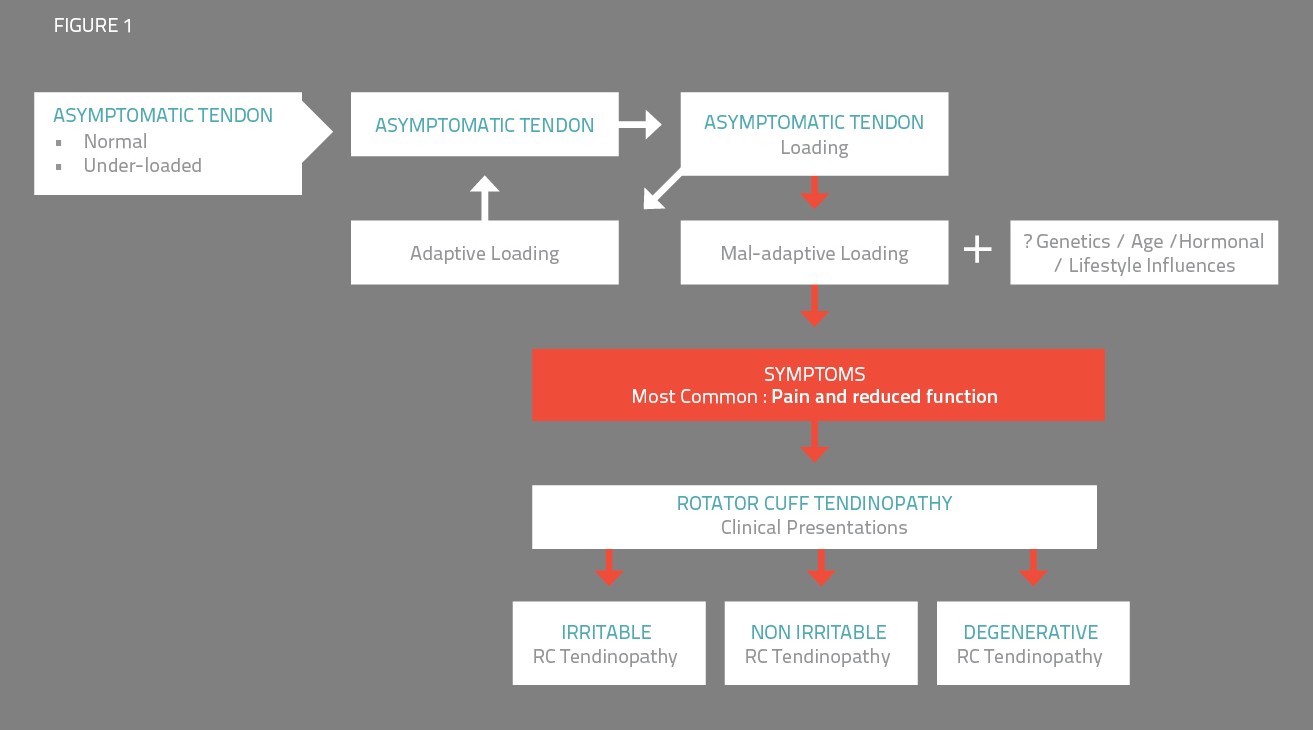
Irritable RC tendinopathy
Irritable RC tendinopathy is characterised by combinations of irritability, constant pain, night pain and an inability to reduce 24-hour pain. There may be concomitant subacromial bursal involvement (Santavirta et al 1992). As with all stages of RC tendinopathy, load management in the form of relative rest is the focal intervention and drives management. The aim of relative rest is to find a level of activity that does not increase, but rather initiates a reduction in 24-hour pain.
Isometric exercises, most commonly in the direction of external rotation, with a towel or pillow placed between the waist and elbow and performed sub-maximally and just at the onset of pain for up to 30 seconds (three repetitions) may help to reduce pain attributed to RC tendinopathy.
There is limited evidence to support this recommendation (Hoeger Bement et al 2008, Lemley et al 2014) and research is currently being conducted to investigate the clinical benefit of this anecdotal observation. The duration, intensity and number of contractions may be varied according to the individual’s response. If contributing to a measure of symptomatic relief, this procedure may be repeated throughout the day, anecdotally and on average up to five times. If the symptoms settle, then a graduated exercise programme may be introduced. In cases where the symptoms are not settling, injection therapy may be considered. Although evidence is equivocal, injections that target the bursa may be associated with a more effective clinical response (Henkus et al 2006).
Following provocative fatiguing activity, people diagnosed with RC tendinopathy demonstrate swelling in the supraspinatus tendon and a reduction in the acromiohumeral distance (McCreesh et al 2014). The swelling may be driven by an increase in tenocytes (Cook & Purdam 2009) and an increase in tendon water content. Both glucocorticoids and selected analgesics have been shown to reduce tenocyte proliferation (Carofino et al 2012; Scherb et al 2009) and injection therapy embedded within RC tendon management, primarily when the presenting symptoms suggest irritability or an inability to cope with exercises due to substantial pain provocation, together with relative rest, may be more appropriate at this stage than it would be in the more degenerative stage where reduced tenocyte numbers are probable (Cook & Purdam 2009).
As discussed, surgery for subacromial impingement syndrome and RC tears has exponentially increased. Research has reported that, following subacromial decompression, non-manual workers may take from nine days to six weeks to return to work, and for manual workers this increases to between three to 12 weeks. Driving is resumed between 13 to 29 days (McClelland et al 2005; Charalambous et al 2010). It is conceivable that one of the benefits of surgery is an enforced period of relative rest followed by a slow, careful and graduated rehabilitation programme which may promote tendon homeostasis. Research comparing a slow incremental rehabilitation programme with and without surgery would be of benefit to understand this possible relationship.
Research has already suggested that people who have failed RC tear repairs may be pain free and their outcome may not differ significantly from those with an intact repair (Kim et al 2012, Slabaugh et al 2010). In addition, it is important to establish the role of placebo in these operative procedures. Moseley et al (2002) reported that there was no difference in outcome between arthroscopic lavage, arthroscopic debridement, and skin incision (placebo) in 180 people undergoing treatment for painful osteoarthritis of the knee, and Sihvonen et al (2013) reported no difference between arthroscopic repair versus placebo surgery for people diagnosed with a painful degenerative tear of the medial meniscus. Similar research is required for both subacromial decompression and RC repair surgery.
Non-irritable RC tendinopathy
When the irritability has settled, or if the individual presents with non-irritable symptoms, the rehabilitation programme is progressed. This should include scapular muscle exercises and a graduated programme of exercises for the RC and may include combinations of flexion, extension, abduction and rotation. The posterior RC (supraspinatus, infraspinatus and teres minor) have been shown to demonstrate increased activity during flexion (Wattanaprakornkul et al 2011a, 2011b), possibly in an attempt to control anterior translation of the humeral head on the glenoid fossa during flexion. Shoulder extension increases the activation of subscapularis. External rotation should be graduated to include unsupported rotation at 90 degrees of abduction.
Progressing exercises to permit pain during the exercise sets may be relevant, as one study specifically permitted and recommended pain up to a level of 5 out of 10 (where 10 represented maximal pain) during the exercise programme, provided that the pain had settled by the next exercise session (Holmgren et al 2012). Activities that require rapid adjustments in balance, assessment and re-assessment of distance to target (where the individual and / or target may be moving), such as playing tennis, baseball and cricket, necessitate that the rehabilitation programme incorporates substantial sensory-motor training. It is also necessary for energy to be transferred from the lower limbs to the shoulder, for example more than 50% of the effort involved in a tennis serve involves energy transfer (Kibler 1995). An important part of shoulder assessment is an evaluation of lower limb and truck range of movement, strength and endurance relevant to the individual’s sport or vocational activity. Any deficits identified need to be included in treatment planning and management.
Education
Appropriate patient education is an integral component of management. People suffering from RC tendinopathy need to appreciate that treatment requires the same respect as a bone fracture. It would be inconceivable to run on a fractured femur or hammer nails into walls with a fractured humerus. While immobilisation is required for a fracture, it is not required for RC tendinopathy, but relative rest and a graduated rehabilitation programme is essential. Discussion focussing on how the individual would cope with work or sport with a recent fracture may help identify solutions for activity modification with RC tendinopathy. Lifestyle issues such as smoking, stress reduction, appropriate nutrition and adequate sleep need to be addressed (Dean & Söderlund In Press-a, In Press-b) by the appropriate member of the healthcare team in a timely manner. The importance of generalised musculoskeletal fitness needs to be emphasised. Keeping a record of activity and responses, most notably the 24-hour response, will assist the patient and therapist to understand the type and amount of loads that are tolerated and will inform exercise and activity progression. For some individuals exercise tolerance for RC exercises may be limited to one set per day, every three days. This does not imply that all components of management would be equally reduced.
Outcomes
As mentioned, clinicians as well as people suffering RC tendinopathy should derive considerable confidence that an exercise approach should achieve the same outcomes as surgical management. Surgery has not demonstrated additional benefit for RC tendinopathy at one, two or five-year follow up (Haahr et al 2005; Haahr & Andersen 2006; Ketola et al 2009, 2013). One study has demonstrated that a graduated exercise programme substantially reduces the need for surgery for up to 80% of people who have already had failed non-surgical treatment (Holmgren et al 2012). For people diagnosed with atraumatic partial thickness tears of the supraspinatus tendon involving less than 75% of the tendon, a graduated physiotherapy exercise programme was as beneficial as surgery involving acromioplasty, or acromioplasty and RC repair (Kukkonen et al 2014). This finding suggests that attempting surgical repair of a RC tear may not improve outcome over a well-structured physiotherapy exercise programme.
Additionally, at two-year follow up, 75% of people diagnosed with an atraumatic full thickness tear and had undergone a graduated exercise programme did not require surgical intervention (Kuhn et al 2013).The findings of these studies suggest that a carefully planned and graduated exercise programme should achieve the same outcomes as surgery for subacromial pain / impingement syndrome, RC tendinopathy (Holmgren et al 2012) partial (Kukkonen et al 2014) and full thickness (Kuhn et al 2013) atraumatic RC tears.
Of importance and relevance to clinicians translating the findings of research to inform clinical practice, as well as department managers, clinical leads and health funding bodies, the number of treatments required to achieve the outcomes reported in these studies ranged from six to 19. This must be considered when offering patients appropriate and evidence based management.
Conclusion
RC tendinopathy is common and is frequently associated with substantial pain and loss of function. A diagnosis of RC tendinopathy is often reached after exclusion of other causes of shoulder pain. This is due to the lack of diagnostic accuracy of the clinical orthopaedic special tests and because structural failure identified by imaging investigations does not always correlate with symptoms. Both clinicians and people suffering with the symptoms of RC tendinopathy should derive considerable confidence that the outcomes achieved with an appropriately graduated exercise programme are equal to those achieved with surgery for RC tendinopathy, and atraumatic partial and full thickness RC tears. Education is an essential component of rehabilitation. Outcomes may also be enhanced by sub-grouping RC tendinopathy presentations and directing treatment strategies according to the clinical presentation as against a generic “one size fits all” approach. Outcomes may be further enhanced by considering the influence of the musculoskeletal chain on shoulder function as well as lifestyle influences. There are substantial deficits in our knowledge regarding RC tendinopathy that need to be addressed to further improve clinical outcomes.
About the author
Dr Jeremy Lewis works in the NHS as well as at the Centre for Health & Human Performance (www.chhp.com), assessing and treating people with often complex shoulder problems. Jeremy has trained as a sonographer (University of Leeds) and performs ultrasound guided shoulder injections, (including hydro-distension procedures for frozen shoulder) as part of the rehabilitation process if required and appropriate. He has an MSc (Manipulative Physiotherapy), and Postgraduate Diplomas in Sports Physiotherapy (Curtin), and Biomechanics (Strathclyde). Jeremy regularly lectures and teaches internationally on the shoulder (www.LondonShoulderClinic.com). In addition to his own research, he supervises PhD and MSc students. Jeremy is an associate editor for the journals Shoulder & Elbow and Physiotherapy. He was a co-editor and author for Grieve’s Modern Musculoskeletal Physiotherapy (4th ed).
Contact Details
Website: www.LondonShoulderClinic.com
Email: jeremy.lewis@LondonShoulderClinic.com
Click here to read the full article

